Medical Device Corrosion Resistance For Ethylene Oxide vs. Gamma Irradiation Sterilization
What is sterilization, and why is it essential for sterile products?
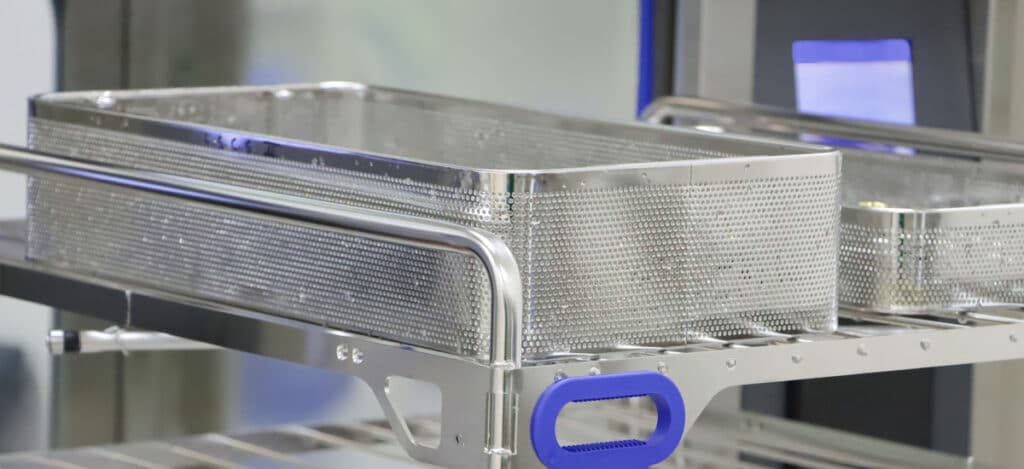
Sterilization (like gamma sterilization or steam sterilization) keeps patients safe from toxins and microbial illnesses when therapies or devices are consumed or used. Sterilization is any process that removes, kills, or deactivates all forms of life. Under the strictest definition of sterility, an item or product is sterile when there is the complete absence of viable microorganisms (bacteria, yeasts, viruses, and molds). Regulatory bodies define sterility by acceptance criteria based on calculated contamination probability for regulatory purposes. An acceptable contamination risk for most items is the probability of a single contaminated product out of a million manufactured products. However, sterility criteria may be more stringent or lax depending upon the intended use of the medical device or product. For reusable medical devices, products must be both sterile and able to withstand multiple sterilization treatments without device corrosion, such as crevice corrosion or microbial induced corrosion. Thus, reusable medical device companies should consider microbial inducted corrosion testing (corrosion testing) along with sterility testing to prove corrosion resistance for their product.
What are the top medical device sterilization methods?
There are seven primary methods for medical device sterilization. These methods are steam sterilization, radiation sterilization, dry heat sterilization, sterilization by filtration, gas sterilization (such as ethylene oxide sterilization), vapor sterilization, and liquid sterilization. Of these sterilization methods, gas sterilization, vapor sterilization, and liquid sterilization techniques are chemical sterilization processes. As you might expect, steam and dry heat sterilization are thermal sterilization processes.
Why is corrosion an issue for reusable medical device sterilization?
Cleaning and sterilization techniques for medical device reprocessing are harsh and can wear on metallic materials over time, resulting in oxidative corrosion. More frequently, the FDA and reusable medical device users want to know how often a device can be reprocessed (cleaned and sterilized) before corrosion occurs. Corrosion can result from a variety of sources such as microbial induced corrosion, crevice corrosion, and cleaning agent corrosion. For this reason, medical device companies should consider corrosion risk during the medical device material selection process.
What is ethylene oxide sterilization?
Ethylene oxide (EO or EtO) is a gas commonly used to chemically sterilize medical devices and products. Ethylene oxide is a potent and highly penetrating alkylating agent. These characteristics make it an extremely effective sterilizing agent. However, at certain levels, ethylene oxide is also capable of causing cancer. Sterilization by ethylene oxide kills microorganisms through exposure to ethylene oxide gas under vacuum and humidity. EtO is used either as one hundred percent EtO, a carbon dioxide mixture, or a mixture with other gasses. As an alkylating agent, ethylene oxide can exacerbate the risk of microbial induced corrosion or crevice corrosion for reusable medical devices after a certain number of cleaning and sterilization cycles. Indeed, alkylating agents like ethylene oxide can alter the properties of materials over time and exposure, leading to an increased risk of crevice corrosion during cleaning or during post-cleaning sterilization. Material properties may also be modified such that microbes readily attach to the reprocessed devices, resulting in a risk of microbial induced corrosion.
How common is ethylene oxide sterilization?
Approximately 20 billion medical devices are sterilized with ethylene oxide each year. Thus, ethylene oxide sterilization accounts for about half of sterilized medical supplies in the United States.
What is gamma sterilization?
Gamma is a radiation sterilization method that destroys the DNA of any live microbes. The mechanism of microbial DNA destruction is called DNA chain cleavage. Gamma rays are highly penetrating and can inactivate microbes with more depth than other radiation methods, such as e-beam beta particles. The thickness and density of a material determine the level of gamma penetration. Gamma radiation penetrates deep into materials and may increase the risk of microbial induced corrosion or biofluid-based corrosion and lead to crevice corrosion in hard-to-reach areas of reusable devices. While microbial induced corrosion is always a risk, biofluids themselves (blood, bile, sweat, etc.) are also corrosive and can increase the risk of device corrosion, particularly crevice corrosion, if not cleaned immediately.
How common is gamma sterilization?
Gamma sterilization is the most popular form of radiation sterilization. However, gamma sterilization is less popular than ethylene oxide sterilization as it is trickier to use for device reprocessing and can break down some heat-sensitive plastics over time.
What products or medical devices can undergo ethylene oxide sterilization?
Due to its low-temperature conditions, ethylene oxide sterilization is well suited for medical devices with embedded electronics and medical devices that cannot withstand steam (autoclave) sterilization. Ethylene oxide is also used to sterilize the personal protective equipment and drapes used by doctors and healthcare workers. Medical devices sterilized with ethylene oxide range from external wound dressings to implantable stents. Other devices include heart valves, vessel closure devices, catheters, and guidewires. Products combining devices, drugs, and biologics within a single item may also be sterilized using ethylene oxide. Ethylene oxide can sterilize almost every type of plastic. Standard materials sterilized with ethylene oxide are plastics, heat-labile materials (e.g., electronics), elastomer polymeric materials, and biomaterials.
Due to the vacuum used during sterilization, ethylene oxide is not recommended for medical devices with embedded batteries. Ethylene oxide sterilization is not recommended for materials sensitive to temperatures ranging from 30°C to 60°C or for medical devices made with materials that are sensitive to humidity. Polymers that are resistant to ethylene oxide sterilization are polyolefin resins such as polypropylene (PP), high-density polyethylene (HDPE), and low-density polyethylene (LDPE).
What products or medical devices can undergo gamma sterilization?
Gamma radiation can easily be used on many materials. However, gamma sterilization is incompatible with polyvinyl chloride (PVC), acetal, and polytetrafluoroethylene (PTFE). If your device contains the polymers listed above, avoid using gamma sterilization to help prevent rapid material degradation and crevice corrosion.
Standard devices and materials sterilized with gamma radiation are plastics, heat-labile materials, glass, and powders. Gamma is generally used to sterilize disposable medical equipment, medical devices, and implants such as arteriovenous shunts, peritoneal dialysis sets, aortic valves, peripheral vascular prosthesis, dental implants, and artificial eyelids. Radiation damages the nucleoproteins of microorganisms, and thus, gamma sterilization is not recommended for most biologics. However, certain devices with microspheres, liposomes, or monoclonal antibodies may be sterilized with gamma.
How is ethylene oxide sterilization performed?
Ethylene oxide sterilized products are placed within an EtO sterilization device. Ethylene oxide sterilization devices look like autoclaves and are enclosure systems that regulate temperature, pressure, humidity, airflow, and EtO gas exposure. Traditional EtO sterilization methods may use EtO-carbon dioxide mixtures with an 8.5% concentration of EtO or EtO-hydrochlorofluorocarbons mixture of 8.6-10% EtO. In some instances, high pressures of 29 pounds per square inch (psi) gauge are needed for sterilization protocols. Resting times for EtO sterilization range from 1-6 hours, and humidity ranges from 40-80%. With EtO sterilization, gas concentration can be increased to reduce EtO processing time.
How is gamma sterilization performed?
Products are sterilized with gamma rays using radiation conveyors. The self-disintegration of Cobalt-60 (60Co) or Cesium-137 (137Cs) creates gamma rays for sterilization. The total radiation dosage is distributed throughout the conveyor system so that there is no change in dose over time. Thus, gamma sterilization applied dosage is adjusted by altering conveyor speed. Gamma radiation effectiveness is dependent on the radiation dosage (absorbed dose) and exposure time. A 12-D sterilization overkill approach is often used for gamma sterilization. The 12-D stands for providing a radiation dose sufficient to produce a 12-log reduction in the D-value of the most resistant microbial spore. A 12-D radiation dosage of 25 mRad is common, as this dosage is greater than 12-fold the D value of B. pumulis. Gamma dosage is verified utilizing dosimeters stationed at various points throughout the radiation sterilization conveyor. Gamma sterilization processing time is much faster than ethylene oxide and is on the scale of minutes vs. hours.
How do ethylene oxide and gamma irradiation corrosion rates compare?
In a 2018 study published in the Journal of Biomedical Materials Research, ethylene oxide (EtO) and gamma irradiation (GI) were compared for their impact on the corrosion rate of four Mg-based materials in CO2 -bicarbonate buffered Hanks’ solution. High-purity (HP)-Mg, ZE41, ultra-high purity (XHP)-Mg, and XHP-ZX00 materials were assessed. The corrosion rate was measured through mass loss and hydrogen evolution. After a two-way analysis of variance (ANOVA) was conducted, neither sterilization technique (ethylene oxide or gamma) significantly influenced the corrosion rate for all four materials examined. P-values for mass loss and hydrogen evolution were (p < 0.84) and (p < 0.08), respectively. This result was consistent across the four materials assessed. Further, there was no interaction between the test variables of the device material and sterilization condition for mass loss (p < 0.49) or hydrogen evolution (p < 0.27). Thus, ethylene oxide or gamma are suggested sterilization techniques for magnesium-based reusable medical devices. Further, magnesium-based materials should be considered when designing your next reusable medical device. While magnesium-based materials are durable and easy to sterilize, biofluids should still be removed as soon as possible during reprocessing to prevent crevice corrosion or microbial induced corrosion.
What is ethylene oxide residuals testing for ethylene oxide sterilization?
The primary issue with using ethylene oxide for sterilization is its absorption into certain materials and its reaction with water or other material components to form toxic residual compounds (ethylene oxide, ethylene glycol, and ethylene chlorohydrin). These residual compounds are hazardous both to people and to the environment. Ethylene glycol is formed from ethylene oxide and water reaction, while ethylene chlorohydrin is formed from the interaction of ethylene oxide and chloride compounds. Products sterilized with ethylene oxide must meet strict ethylene oxide residual limits to keep patients safe during medical device and product use. Current ISO 10993-7 ethylene oxide residual limits can be found here.
Summary
Overall, reusable medical devices and products must be sterile and corrosion-resistant during reprocessing. Sterilization is any process that removes, kills, or deactivates microbes. Ethylene oxide gas is used to kill organisms for EtO sterilization. Gamma is a form of radiation sterilization that utilizes ionizing radiation to inactivate microbes. Both gamma radiation and ethylene oxide are commonly used to sterilize heat-sensitive devices. In terms of corrosion, ethylene oxide sterilization and gamma sterilization were found to have the same corrosion rate for magnesium-based materials. Indeed, EtO and gamma sterilization did not significantly influence the corrosion rates of magnesium-based medical implants and devices. Thus, either EtO or gamma are reliable sterilization methods for magnesium-based reusable medical devices. Further, magnesium-based materials should be considered when designing your next reusable medical device. All in all, ensure you choose a contract testing organization that can provide appropriate corrosion testing, cleaning validations, sterility testing, and ethylene oxide residuals testing for your product needs.
MycoScience is a contract manufacturing organization specializing in sterile syringe and vial filling for parenteral products. MycoScience also offers testing services, including Preservative Efficacy Testing/Suitability Testing, Bioburden Testing, Microbial Aerosol Challenge Testing, Cytotoxicity Testing, Cleaning Validations, Accelerated Aging, Microbiology Testing, EO Residual Testing, Bacterial Endotoxin Testing, Package Integrity Testing, Sterilization Validations & Environmental Monitoring services medical devices and allied industries. MycoScience is an ISO 13485 certified facility.
References
Bernhard Linke. Sterilization methods and impact on electronics in medical devices. EE Times. July 2011.
Byron J. Lambert, Todd A. Mendelson & Michael D. Craven. Radiation and Ethylene Oxide Terminal Sterilization Experiences with Drug-Eluting Stent Products. AAPS PharmSciTech. Vol. 12: 1116–1126. 2011.
Center for Disease Control. Ethylene Oxide “Gas” Sterilization: Guideline for Disinfection and Sterilization in Healthcare Facilities. Article. 2008.
International Organization for Standardization. Biological evaluation of medical devices — Part 7: Ethylene oxide sterilization residuals. Geneva (Switzerland): ISO; 2008. (ISO 10993-7:2008).
Michael J. Akers. Sterile Drug Products Formulation, Packaging, Manufacture, and Quality. Drugs and the Pharmaceutical Sciences. Informa Healthcare. 2010.
Purell. Sterilization Of Polyolefins: A Methodological Overview. Lyondell Basell Industries.2011.
Sean Johnston, et al. The influence of two common sterilization techniques on the corrosion of Mg and its alloys for biomedical applications. Journal of Biomedical Materials Research. 106(5):1907-1917pg. 2018.
United States Food & Drug Administration. Ethylene Oxide Sterilization for Medical Devices. Digital Article. September 2020.
United States Pharmacopeial Convention. <1211> Sterility Assurance. Rockville, MD, USA. 2021. (USPC <1211>).
United States Pharmacopeial Convention. <1229> Sterilization of Compendial Articles. Rockville, MD, USA. 2021. (USPC <1229>).
United States Pharmacopeial Convention. <1229.10> Radiation Sterilization. Rockville, MD, USA. 2021. (USPC <1229.10>).
Sharing this in your social netwroks

