Preservative Efficacy Testing Vs. Sterility Testing
What are preservatives?
Preservatives are substances mixed into creams, gels, and other liquids. Preservatives are used to prevent the growth of bacteria, fungi, and other microorganisms within a medical, cosmetic, household, or food product. Preservatives also help keep the freshness of the appearance of a product and keep its consistency intact over time. A USP preservative efficacy test can evaluate how well a preservative inhibits microbial growth. USP preservative efficacy test is often paired with USP sterility testing for the product and product packaging. When outsourced, rapid sterility testing can be obtained along with preservative efficacy testing.
What is preservative efficacy testing (PET)?
Preservative efficacy testing, also known as preservative challenge testing, determines the effectiveness of a preservative during its shelf life and evaluates how well a product withstands microbial contamination during use.
What is sterilization, and why is it essential for sterile products?
Sterilization keeps patients safe from toxins and microbial illnesses when therapies or devices are consumed or used. Sterilization is any process that removes, kills, or deactivates all forms of life. Under the strictest definition of sterility, an item or product is sterile when there is the complete absence of viable microorganisms (bacteria, yeasts, viruses, and molds). Sterility is defined by regulatory acceptance criteria based on calculated contamination probability. An acceptable level of contamination risk for most items is the probability of a single contaminated product out of a million manufactured products. However, sterility criteria may be more stringent or lax depending upon the intended use of the medical device or product. Common sterilization processes utilize chemicals, heat, radiation, or filtration. Radiation sterilization is one of the fastest sterilization methods and often provides a rapid sterility testing turnaround for sterilization validations.
What is sterility testing?
USP sterility testing evaluates a product for live microbes and ensures that microbes have been appropriately excluded or destroyed. Microbes can be excluded through aseptic processing or effectively killed through terminal sterilization methods. A component of USP sterility testing is sterilization process validation. Sterilization validations are used to ensure that the end sterilization process can appropriately kill any viable microorganisms in a sample. The most popular method for sterilization validation is an overkill method.
What products require preservative efficacy testing?
Preservative efficacy testing can be used to determine the best preservative to use in your topical formulation and the minimum effective concentration needed to preserve the pharmaceutical, food, or biotechnology product being assessed. Topical formulations (gels, creams, ointments, and lotions) comprise a water or oil base that delivers various medications, natural substances (such as herbs), or moisture through the skin. Topical cosmetics contain preservatives to support the stability of the formulation and prevent microbial growth during repeated product use. Preservative challenge testing is also used for parenteral products containing multiple doses. In these products, antimicrobial preservatives inhibit the growth of any microorganisms introduced during repeated insertion and withdrawal to load individual amounts.
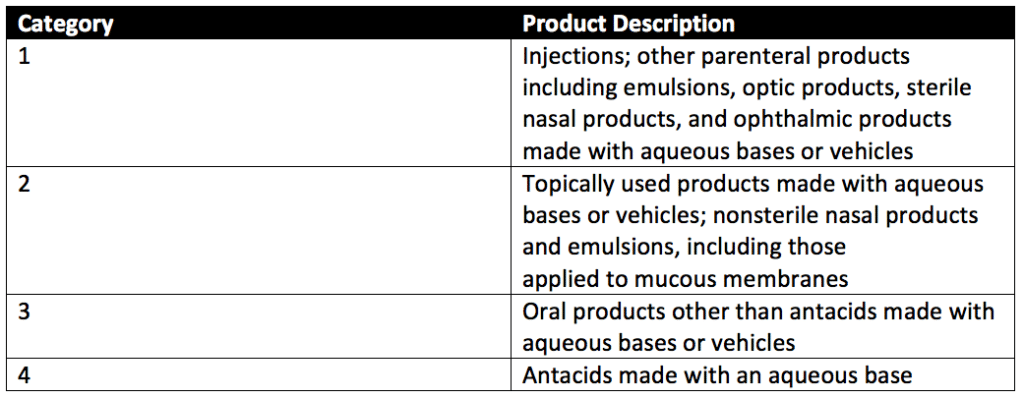
USP preservative efficacy testing can evaluate four categories of products with preservative challenge testing. These product categories are detailed in Table 1 of USP 51, reproduced below.
What products require USP sterility testing?
All sterile products and products that undergo terminal sterilization processes require USP sterility testing to prevent product-induced illness. Thus, many medical device, drug, and cosmetics companies seek options for rapid sterility testing.
How is preservative challenge testing performed?
Three approaches are used in preservative challenge testing. These approaches come from the Schülke KoKo Test, United States Pharmacopeia (USP), and the European Pharmacopeia.
Schülke KoKo Test vs. U.S. Pharmacopeia vs. European Pharmacopeia
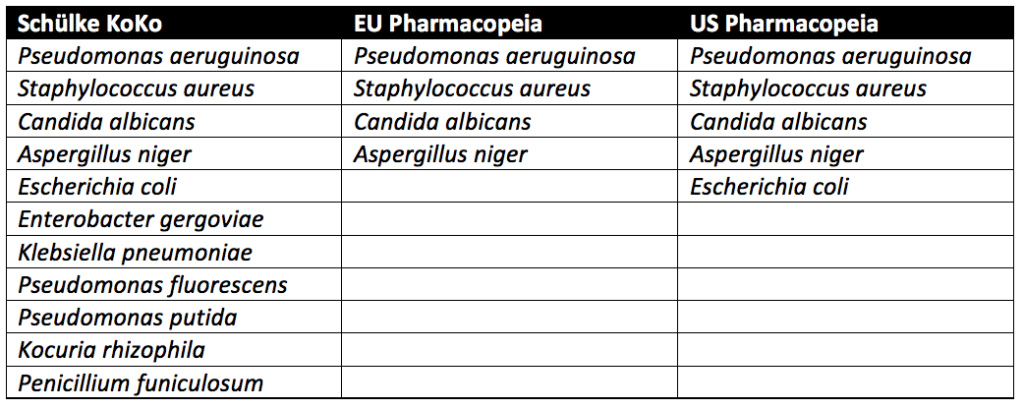
Pseudomonas aeruginosa, Staphylococcus aureus, Aspergillus niger, and Candida albicans must be tested for in all cosmetic products sold in the European Union. In addition to the microbes above, testing with microbes known to lead to spoilage of cosmetic products is recommended but not required. In the United States, the USP guidelines require testing of Escherichia coli in addition to Pseudomonas aeruginosa, Staphylococcus aureus, Aspergillus niger, and Candida albicans. Spoilage microbes are not needed for PET. In contrast to the pharmacopeia tests, which only evaluate pathogenic microbes, the Schülke KoKo test evaluates product spoiling microorganisms. Schülke KoKo test’s spoiling microorganisms are based on decades of cosmetic testing experience from Schülke & Mayr in Germany.
USP preservative efficacy testing evaluates cosmetic products by exposing them to a single microbial strain at a time. Additional details on USP preservative challenge testing, which follows similar procedures to the European Pharmacopeia, can be found through reading our articles on Preservative Challenge Testing And USP 51 and Preservative Efficacy Testing For Medical Devices. In contrast, for the Schülke KoKo test, the single cultivated microbes are brought together into a mixed suspension to challenge the cosmetic product. A new mixed suspension is prepared for each of the six inoculation cycles for Schülke KoKo testing. Since the Schülke KoKo test uses a mixed microbe inoculation, it simulates microbial exposure of a product during production, filling, and use. Indeed, a product would likely be exposed to multiple microbes at once instead of one at a time. Overall, though different from the USP and European Pharmacopeia methods, the Schülke KoKo Test is a reliable test method for assessing the efficacy of antimicrobial preservation of cosmetic products.
First, cultures of Candida albicans (ATCC No. 10231), Aspergillus brasiliensis (ATCC No. 16404), Escherichia coli (ATCC No. 8739), Pseudomonas aeruginosa (ATCC No. 9027), and Staphylococcus aureus (ATCC No. 6538) are prepared. Stock cultures of these organisms are prepared by centrifuging an ATCC culture removing residual media from the prior culture and resuspending the microorganisms in a sterile suspension fluid. The suspension fluids for each microorganism referenced above are prepared at a microbial count of about 1 × 108 colony-forming units per milliliter (CFU/mL).
Preservative efficacy testing is performed in five sterile, capped containers. Suppose the product’s original container is sterile, can be entered aseptically, and holds an appropriate product volume. In that case, the original filled product containers may be used. Each of the five product samples is injected with a test suspension of either Candida albicans, Aspergillus brasiliensis, Escherichia coli, Pseudomonas aeruginosa, or Staphylococcus aureus. Each product sample is exposed to only a single microbe of the five listed, and all microbes are exposed to the product during testing. The microbial test suspension injected is between 0.5%- 1% of the volume of the product under assessment and is at a concentration of 1 × 105 and 1 × 106 CFU/ml of the product for category 1-3 products. The final concentration per ml of category 4 products is between 1 × 103 and 1 × 104 CFU/mL.
Each of the five product samples with their respective microbial injections is incubated at a simulated room temperature of 22.5 ± 2.5°C or 32.5 ± 2.5°C depending upon the microbe the product sample is exposed. Microbial counts are taken at 7, 14, and 28 days for most microorganisms tested. The plate-count method determines the number of CFU present in each inoculated product sample. This plate-count method is completed in duplicate. Once all counts are taken, the change in log10 of the concentration of CFU/ml is calculated for each microorganism. The requirements for antimicrobial effectiveness are met if no increase in microbial growth for the various organisms tested occurs within the timeframes specific to each organism. are met. No increase in microbial growth is defined as not more than 0.5 log10 units more than the previous microbial growth value.
How Is USP sterility testing performed?
Sterile processes must have a one in a million probability of unit contamination (or less) to pass sterilization validation acceptance criteria. Sterility acceptance criteria are also known as sterility assurance levels (SALs). Sterilization validations for microbial inactivation processes can be performed via three techniques: overkill methods, bioburden-biological indicator methods, and bioburden-based methods. All three techniques are equally accurate. The overkill method is the simplest. However, it is the most stressful for sterilized materials. The bioburden-based method requires the greatest method control but allows sterilized materials to undergo the least stressful conditions. All three sterilization validation techniques are described in greater detail below.

#1: Overkill Sterilization Validation Method
Due to its simplicity, the overkill method is preferred for rapid sterility testing of medical devices and items unaffected by the sterilization processes. Items that could be damaged by extended sterilization process exposure should not be assessed via an overkill method. With an overkill method, the destruction of a high concentration of resistant microorganisms (bacterial spores) supports killing the bioburden present during normal medical device or item sterilization. An overkill validation is passed if any of the following criteria are met: a defined minimum lethality, a defined set of method conditions, or confirmation of minimum log reduction of a resistant biological indicator. Overkill sterilization validations are governed by ISO 17655-1.
#2: Bioburden-Biological Indicator (Combination) Sterilization Validation Method
A combination bioburden-biological indicator sterilization validation is an approach where the partial destruction of a resistant biological indicator can be used to demonstrate the ability of the sterilization process to reliably destroy the routine bioburden present during medical device (or product) sterilization. A combination approach requires detailed knowledge of the anticipated product bioburden, biological indicator populations, and the relative resistance of the anticipated bioburden and biological indicator populations.
#3: Bioburden-Based Sterilization Validation Method
The bioburden-based method is used when material stability is poor or when no suitable biological indicator microorganisms are available for sterilization. Traditionally, radiation sterilization processes are validated using a bioburden-based method. In a bioburden-based method, bioburden samples from the device or product are routinely evaluated for resistance to the sterilization process. Lack of device resistance to the sterilization process can then be utilized to demonstrate its effectiveness. For this sterilization validation method, routine monitoring of the product bioburden population (and any resistance to the sterilization process) is required. Using a contract testing company for rapid sterility testing that is familiar with environmental monitoring is advantageous for bioburden-based sterilization validations.
What are the differences between preservative efficacy and sterility testing?
Sterility process validations and testing are quality control steps for verifying the effective removal or destruction of live microorganisms from medical products. Only living microorganisms are of concern for the sterility of medical products since only live microorganisms have the potential to reproduce in the human body, on the medical product surface, or within the medical product itself to cause sickness or disease. In contrast, preservative challenge testing determines the best preservative for use and the minimum effective concentration needed to preserve multidose parenteral products, topicals products, food, or other healthcare items that contain preservatives. Together preservative efficacy and sterility tests ensure that parenteral products, cosmetic products, and medical devices meet the regulatory criteria for sterility and antimicrobial activity.
Summary
Overall, preservative efficacy testing (PET) and sterility testing are imperative for the regulatory approval of pharmaceuticals, cosmetics, and medical devices. These tests ensure that parenteral products, topicals, and medical devices have appropriate antimicrobial protection and maintain their sterility overtime to keep patients safe during product use. All in all, ensure you choose a contract manufacturing organization that can support you with rapid sterility testing and preservative efficacy testing for your unique cosmetic, pharmaceutical, or medical device product needs.
MycoScience is a contract manufacturing organization specializing in Preservative Efficacy Testing, Sterilization Validations and sterile syringe and vial filling. MycoScience also offers Bioburden Testing, Cleaning Validations, Microbial Aerosol Challenge Testing, Accelerated Aging, Microbiology Testing, Cytotoxicity Testing, Bacterial Endotoxin Testing, EO Residual Testing, Package Integrity Testing & Environmental Monitoring services medical devices and allied industries. MycoScience is an ISO 13485 certified facility.
References
International Organization for Standardization. Sterilization of health care products- Moist heat- Part 1: Requirements for the development, validation, and routine control of a sterilization process for medical devices. Geneva (Switzerland): ISO; 2006. (ISO 17665-1:2006/(R)2016).
Michael J. Akers. Sterile Drug Products Formulation, Packaging, Manufacture, and Quality. Drugs and the Pharmaceutical Sciences. Informa Healthcare. 2010.
United States Pharmacopeial Convention. <51> Antimicrobial Effectiveness Testing. Rockville, MD, USA. 2021. (USPC <51>).
United States Pharmacopeial Convention. <1211> Sterility Assurance. Rockville, MD, USA. 2021. (USPC <1211>).
United States Pharmacopeial Convention. <1229> Sterilization of Compendial Articles. Rockville, MD, USA. 2021. (USPC <1229>).
Sharing this in your social netwroks

